Our Care Strategy

Since 1957, the Parkinson’s Foundation has been a national leader in improving care for people with Parkinson’s disease (PD). We drive a multi-disciplinary care strategy to advance our vision that every person with Parkinson’s receives the highest quality care possible, regardless of setting.
We Are Improving Care
Our key care priorities are to:
- Define quality Parkinson’s care across the care continuum.
- Empower people with Parkinson’s to advocate for timely, quality and person-centered care that aligns with their goals.
- Support education and training of a robust Parkinson’s care network and workforce to deliver quality care to a growing Parkinson’s community.
- Expand the evidence base for emerging best practices, care models and tools to accelerate dissemination.
We are committed to working with health care, government, researchers, and most importantly, people with PD and their care partners, to shape a system that is grounded in the needs and priorities of those who live with Parkinson’s.
The Care Crisis
Parkinson’s is the fastest growing neurological disorder in the world. There is no cure. As Parkinson’s prevalence rises in the aging U.S. population, both financial and healthcare systems face significant challenges.
- Nearly one million Americans live with PD. That number is projected to increase to 1.2 million by 2030 as the U.S. population ages.
- Nearly 90% of people with PD are covered by Medicare. The average age of diagnosis is 60 years old, and incidence increases with age.
- In 2019, approximately 808,107 Medicare beneficiaries had a PD diagnosis and almost 40% of those with Medicare and PD were enrolled in a Medicare Advantage plan.
- While age is the prime risk factor, PD affects people of all ages regardless of sex, race, ethnicity, socioeconomic status, or geography.
Professional Education Opportunities
We provide best-practice care training with the latest Parkinson's information. Explore our educational tools for doctors, nurses and every member of the health care team.
Rising Healthcare Costs
As the number of people with PD rises, so too will the associated costs. The combined cost of Parkinson’s, including treatment, social security payments and lost income, is estimated to be nearly $52 billion per year in the U.S. alone and is projected to surpass $79 billion by 2037.
The federal government alone accounts for nearly $25 billion in annual spending on PD care, with $2 billion supported through Social Security and the remaining $23 billion in Medicare costs.
Specialist Shortage
There is a growing shortage of physicians who specialize in Parkinson’s. Today there are only 660 movement disorders specialists (neurologists with advanced PD training) practicing in the U.S. and fewer than 10 practicing in rural areas.
Research shows that the projected supply of neurologists will not meet the growing demand driven by the rapidly aging U.S. population. Estimates show that by 2025 there will be a 19% shortage in the number of needed neurologists.
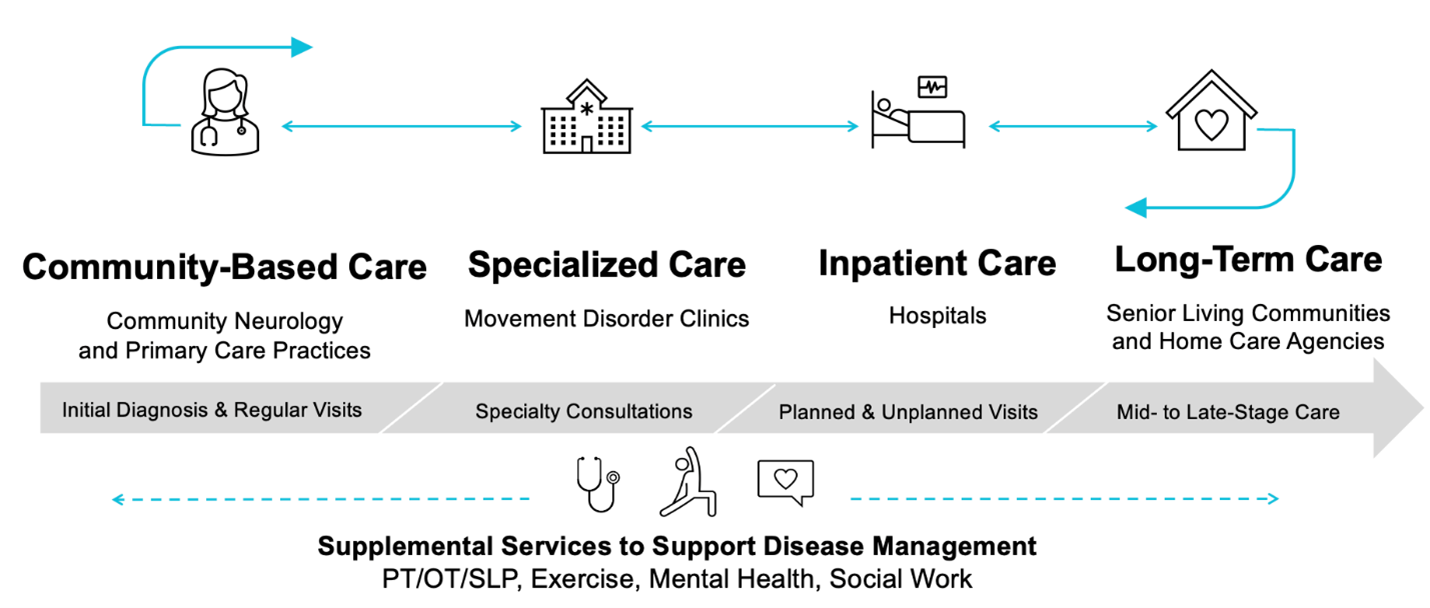
The Parkinson’s Care Continuum
As people navigate Parkinson’s, they will receive care in different settings dependent on factors like current symptoms, treatment plan and availability of specialists.
Optimal PD care involves an interprofessional healthcare team including movement disorder specialists, general neurologists, nurses, nurse practitioners and therapy providers.
The Parkinson’s Care Continuum highlights the varied pathways that people with PD may take as they move between each setting. The Foundation’s care priorities and programs target key partners to address challenges and drive changes across this care continuum.
Quality Parkinson’s Care
Parkinson’s care will look different across the care continuum as a person navigates PD and its stages.
The Foundation has identified five principles of quality Parkinson’s care that will enhance quality of life, mitigate risk of preventable harm, and reduce costs across the care continuum.
These principles are designed as a:
- Baseline for people with PD and their loved ones to assess the care they are receiving
- Guide for health professionals who are providing PD care
- Benchmark for institutions invested in quality improvement.
Principles of Quality Parkinson’s Care
- Early diagnosis and treatment
Timely diagnosis and treatment of Parkinson’s symptoms. - Symptom management
Early referrals to supplemental therapies like physical therapy, occupational therapy, speech language pathology and behavioral health services. - Medication management
Timely medication administration, proper dosing and avoidance of contraindicated medications to optimize health outcomes and prevent symptom deterioration. - Team-based care
Robust care coordination across a bolstered workforce to improve and expand access to patient-centered care. - Person- and family-centered care
Individualized care focused on patient goals and unique disease progression, quality of life and care partner engagement.
Our Care Programs
Community Neurology Initiative
Research from the Parkinson’s Foundation shows that most people with Parkinson’s receive PD care from general neurologists and primary care providers. Our Community Neurology Initiative aims to reach healthcare professionals who are providing neurology care in their communities and connect them with the Foundation’s free resources. We know PD care is demanding; we are here to help.
Global Care Network
The Parkinson’s Foundation recognizes medical facilities around the world for meeting rigorous care criteria. Our Global Care Network creates more opportunities for people with PD to access high-quality care while also providing health professionals the chance to advance and share their knowledge.
Hospital Care Initiative
Each year in the U.S., nearly one-third of people with Parkinson’s will be hospitalized, putting them at increased risk for complications and longer lengths of stay when compared to those without PD. Our Hospital Care Initiative aims to eliminate preventable harm and promote higher reliability in care for people with Parkinson’s in the hospital.
Community Partners in Parkinson’s Care
Up to 25% of people with PD live in senior living communities, but many professionals in this setting lack Parkinson’s training. Our Community Partners in Parkinson’s Care Program educates the staff at senior living communities and home care agencies on optimal care for people with PD.
Palliative Care Initiative
Palliative care addresses physical, social, emotional and spiritual needs to improve the quality of life for a person with Parkinson’s and their family from diagnosis through every stage of the disease. Our Palliative Care Initiative has trained more than 800 health care professional team members who provide care to more than 70,000 people with PD.
Rehabilitation Medicine Initiative
Rehabilitation services — which includes physical and occupational therapy, speech-language pathology and psychology/neuropsychology — can play a crucial role in managing and improving PD symptoms and quality of life from day one. Our Rehabilitation Medicine Initiative aims to raise awareness of the importance of rehabilitation care in PD.